




The Sentara Nursing Experience
Making a meaningful impact on health requires compassion, dedication, continuous learning, teamwork and collaboration. At Sentara, we also recognize that in valuing the professional and personal well-being of our nurses, we build a stronger, more supportive workplace for our nurses. And that’s making us healthier from the inside out. These principles unite our nurses across various roles and locations.


The Sentara Clinical Experience
No matter where you choose to join us, in an inpatient or outpatient setting, you will be part of an interdisciplinary Clinical team passionate about quality care and patient safety. You will have access to the tools and technologies you need to succeed and the chance to learn and grow through training and educational programs so you can advance your career as a Clinical professional.

The Sentara Support Services Experience
Each day, the Sentara Support Services team helps improve healthcare at more than 300 Virginia and Northeastern North Carolina sites. We perform various patient care activities, provide multiple services, and handle administrative functions that support our patients and their families. These vital functions include assisting the medical team in all aspects of medical care, such as treatments, procedures, and diagnostic and laboratory testing.

The Medical Group Experience
As part of Sentara Health, Sentara Medical Group providers have diverse opportunities across regions and inpatient and outpatient locations. For those providers based in one of 12 hospitals, we have close working relationships with the administration, ensuring a collegial and collaborative environment where all can come together around shared initiatives.
Guided by a dedicated board of providers, Sentara Medical Group not only offers leadership opportunities for its providers but also underscores the group’s crucial role in fulfilling Sentara’s overarching mission to meet the needs of our diverse patient populations, some of our most vulnerable communities. Our physicians and APPs enjoy opportunities for both personal and professional career growth through a network of resources aimed to cultivate an environment suitable for a lifelong career home.
Your Perspective Matters
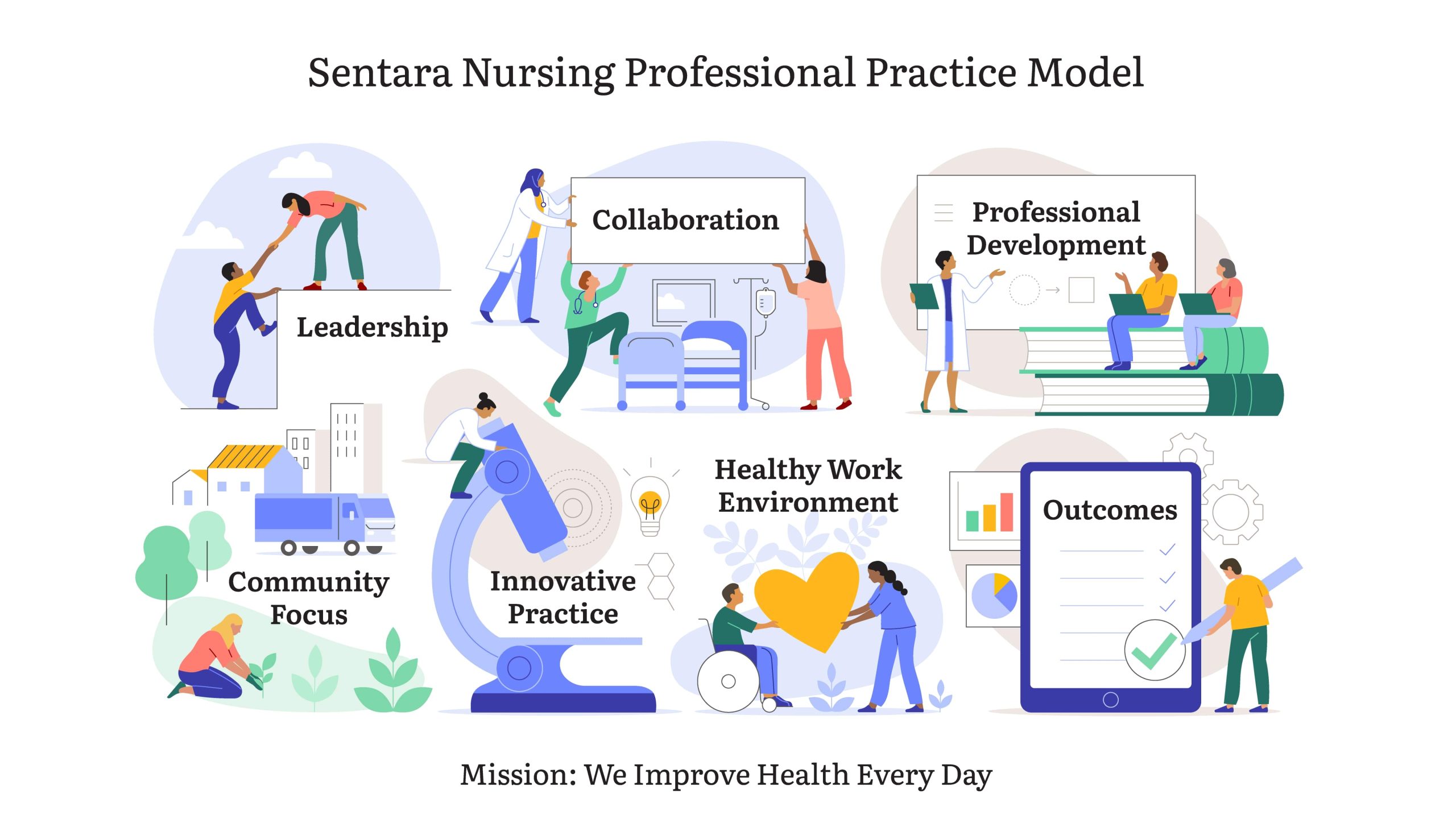
Nurses are the heartbeat of our exceptional team. Our approach empowers nurses to actively participate in decision-making. Our nurses have a stake in shaping their workplace as well as their own career growth; one of the benefits of our focus on supporting and valuing team members. This framework encompasses our nursing mission, vision, values, philosophy, and the essential elements of our Professional Practice Model.
This image illustrates the Sentara Nursing Professional Practice Model. Read more about it on The Sentara Nurse Experience page.
Our Award-Winning Care
We Are an Equal Opportunity Employer
Sentara Health is an Equal Opportunity Employer committed to the hiring, advancement, and fair treatment of every individual. Sentara and its affiliates do not discriminate against any individual or group of individuals on the basis of race, color, religion, ancestry, national origin, marital status, age, sex, sexual orientation, gender identity or expression, genetic information, physical or mental disability, pregnancy, medical condition, veteran status or any other legally protected characteristics.
Similar Jobs
We Are an Equal Opportunity Employer
Sentara Health is an Equal Opportunity Employer committed to the hiring, advancement, and fair treatment of every individual. Sentara and its affiliates do not discriminate against any individual or group of individuals on the basis of race, color, religion, ancestry, national origin, marital status, age, sex, sexual orientation, gender identity or expression, genetic information, physical or mental disability, pregnancy, medical condition, veteran status or any other legally protected characteristics.



























